The 2020 National Average Scores for Plan Reporting Data Validation for reporting year 2019 were released on July 1st after Data Validation submission activities were finalized on June 30th.
So, how did plans fare in the 2020 Data Validation Audits?
Check out the score summary below which is also available on Health Plan Monitoring System’s (HPMS) site, for Part D reporting sections:
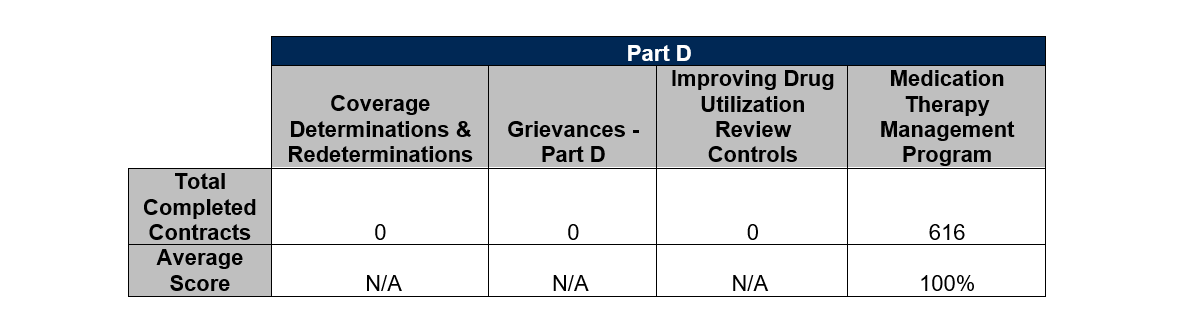
The reporting sections requiring validation and upload for the 2020 Data Validation season were completed with remarkable results! Overall, PillarRx clients performed and exceeded CMS audit standards. Our clients have a strong enthusiasm for the quality and integrity of their compliance programs and reporting, ensuring best practice approaches were implemented on behalf of their members. Year over year, our clients continue to impress our audit staff with their drive to improve and adapt to the changing times and requirements, utilizing our DV services year-round, and working with CMS to obtain better clarity on the reporting sections undergoing validation.
The Medication Therapy Management Program (MTMP) was the only Part D reporting section required to undergo validation this season. The narrowing of reporting sections came about because of the unprecedented circumstances surrounding the COVID-19 public health emergency.
So, why was MTMP selected for validation over all the other Part D reporting sections this season?
The MTM programs purpose is to aid plans, clinicians, and members in producing the best therapeutic outcomes. MTM is made available through all Part D plans for members who have chronic conditions, take multiple medications, and are at risk for spending more money on annual Part D covered drug costs than a certain cost threshold. In 2019 that threshold was set at $4,044. As a reporting section, it also contributes to a plans Star Rating, while the other reporting sections that typically undergo validation do not.
Star ratings are very important and serve in providing comparative information to enrollees as well as identifying whether a plan is eligible for a Quality Bonus Payment (QBP). For this reason, CMS maintained the validation requirement on MTM for the 2020 data validation season.
What are the continued impacts of COVID-19 on CMS quality rating systems like Star Ratings?
This past May, CMS issued a final rule on enhancements to Part C and D programs, specifically regarding the quality rating system. CMS adopted a series of changes in the March 31, 2020, Interim Final Rule with Comment (CMS-1744-IFC) for the 2021 and 2022 Star Ratings due to challenges that have continued to develop from the COVID-19 public health emergency. These changes, “Modify the calculation of the 2021 and 2022 Part C and D Star Ratings to address the expected disruption to data collection and its impact on measure scores posed by the COVID-19 public health emergency to avoid inadvertently creating incentives to place cost considerations above patient safety.”
For Non-CAHPS and Non-HEDIS star rated measures like that of MTM within the Data Validation Audit, CMS has the final determination about the inclusion of measures in each year’s Star Ratings. With the potential for multiple measures to have data quality issues across many plans as a result of COVID-19, CMS is addressing this issue by adopting a rule to permit replacing the 2021 Star Ratings measure scores and stars with the 2020 Star Ratings measures scores and stars for the impacted measures for all plans rather than excluding multiple measures from the 2021 Star Ratings calculations.
For example, when there is a systemic data quality issue for all plans as a result of the COVID-19 public health emergency, CMS will use sponsors’ MTM Program Completion Rate for Comprehensive Medication Review measures’ scores and stars from the 2020 Star Ratings as the sponsors’ 2021 Star Ratings on those measures. This rule adoption, gives authority for CMS to substitute the score and star for the measure used in the 2020 Star Ratings in the calculation of the 2021 Star Ratings.
These Star Ratings enhancements support CMS efforts to increase stability in the program.






Leave A Comment